Software is the central nervous system of modern healthcare. It's the hidden force transforming everything from your personal health records to the precision of robotic surgery. The discipline of software engineering in healthcare is all about designing, building, and maintaining these incredibly complex systems that run hospitals, clinics, and the health apps on your phone.
Honestly, this field is the key to navigating the industry's massive operational hurdles and regulatory minefields. For entrepreneurs and business leaders, getting this right means building applications that are not just innovative but also secure, scalable, and built to last. A key part of modernizing these applications is integrating AI, but this introduces new complexities. Managing AI prompts, controlling API costs, and ensuring model reliability can quickly become a headache. That's where a smart administrative tool, like the prompt management system we've developed at Wonderment, becomes essential for modernizing your app and building it to last for years to come.
Why Software Engineering Is Healthcare's New Heartbeat
Code isn't just a side-tool in medicine anymore; it's the core infrastructure. Think about it. From the moment you book an appointment online to the AI algorithm helping a radiologist spot anomalies on a scan, software is there every step of the way. It helps untangle complex clinical workflows, makes care safer by cutting down on human error, and opens up access through telehealth and mobile apps.
This digital shift is creating a huge demand for skilled engineers. The global healthcare software market is absolutely booming, with over 3,180 companies and 1,770 startups pushing new solutions forward. This sector gives jobs to more than 181,000 people worldwide and added over 17,000 new positions last year alone—that's a solid 10.30% growth rate. This isn't just a trend; software engineering is now essential for delivering effective, sustainable healthcare.
Navigating the Complexity of Modern Healthcare
Building software for healthcare is nothing like building an app for another industry. The stakes are incredibly high. One bug isn't an inconvenience; it could be a serious patient safety issue. The entire environment is governed by strict regulations designed to protect our most sensitive information.
This requires a unique mix of raw technical skill and deep domain knowledge. Developers have to create systems that are not only slick and user-friendly but also relentlessly secure and compliant. It's a huge part of the larger digital transformation in healthcare, where we're finally using technology to solve problems that have plagued medicine for decades.
This is what a modern healthcare software solution looks like—an intricate system designed to meet these exact challenges.
This image perfectly captures how modern software has become the digital heart of healthcare, pumping data and functionality through the entire system to keep it alive and well.
The Next Frontier: AI Integration
The next major leap is baking artificial intelligence directly into these systems to make them smarter. But here’s the catch: adding AI introduces whole new layers of complexity. Juggling AI prompts, keeping API costs from spiraling out of control, and ensuring different models are reliable can quickly become a nightmare for development teams.
A specialized AI management system is the answer. It simplifies all this complexity, letting developers and entrepreneurs build more intelligent healthcare solutions without getting buried in administrative tasks. Think of it as the mission control for AI integration.
Tools built to manage prompts, track costs, and log AI performance are non-negotiable for modernizing applications responsibly. This management layer is what gives innovators the confidence to build, knowing their AI-powered features are scalable, secure, and won't break the bank. It's the final piece of the puzzle for turning a brilliant idea into a successful, long-lasting healthcare application.
Building a Fortress Around Patient Data
In healthcare, patient data isn't just information; it's the most valuable and sensitive asset an organization can have. The job of software engineering in healthcare is to build a digital fortress around that data. A single breach doesn't just tarnish a company's reputation—it can expose people to fraud, compromise their medical care, and trigger devastating legal consequences.
Think of it like building a bank vault. You wouldn't settle for a standard lock. You’d engineer multiple layers of security, from reinforced steel walls and time-locked doors to biometric scanners. In the same way, protecting patient data demands a multi-layered defense, and the absolute foundation of that defense is compliance.
The Ground Rules: HIPAA, GDPR, and More
Before a single line of code is written, you have to understand the rulebook. Regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in Europe are the blueprints for your fortress. They aren't just suggestions; they are legally mandated frameworks that dictate every single detail of how Protected Health Information (PHI) is managed.
These regulations govern everything from data encryption (both in transit and at rest) to implementing strict access controls so only authorized personnel can ever view patient records. Breaches are incredibly costly, with HIPAA violation penalties hitting up to $1.5 million per year for each violation. For a deeper dive, our guide on HIPAA compliant app development breaks down all the essential technical safeguards you'll need.
To build secure and effective healthcare software, it's crucial to understand the landscape of these governing standards. The table below outlines the core regulations and standards that form the bedrock of the industry.
Core Healthcare Data and Compliance Standards
| Standard/Regulation | Primary Purpose | Key Focus Area |
|---|---|---|
| HIPAA | Protects sensitive patient health information in the U.S. | Privacy, Security, Breach Notification, Patient Rights |
| GDPR | Grants data privacy rights to individuals in the European Union. | Data Protection, User Consent, Data Portability |
| HL7 | Enables clinical and administrative data exchange. | Messaging Standards, Data Structuring, Legacy Systems |
| FHIR | Modernizes healthcare data exchange using web APIs. | API-based Interoperability, Mobile Health, Real-time Data |
Navigating these standards isn't just about avoiding fines; it's about building trust and ensuring patient safety is at the core of your technology.
Creating a Universal Language for Health Data
Securing data is one thing, but making sure different systems can understand it is another challenge entirely. A patient's journey often weaves through multiple providers, labs, and pharmacies. Without a common language, critical information gets trapped in silos, leading to medical errors and frustratingly inefficient care. This is where interoperability standards step in.
Think of these standards as a universal translator for healthcare. They allow a patient’s allergy information from their family doctor's system to be instantly understood by an emergency room's system, ensuring they get safe and effective treatment.
Interoperability isn't just a technical feature; it's a patient safety imperative. When systems can communicate seamlessly and securely, it prevents dangerous gaps in a patient's medical history, leading to better diagnoses and coordinated care.
Two primary standards are leading this charge:
- HL7 (Health Level Seven): This is the old guard, the established workhorse that has powered healthcare data exchange for decades. It's the standard for exchanging clinical and administrative data between legacy systems.
- FHIR (Fast Healthcare Interoperability Resources): As the modern successor, FHIR is a web-based standard that’s far more flexible and easier for developers to work with. It's rapidly becoming the new default for building apps that can securely pull and share data from electronic health records (EHRs).
Bringing It All Together in Practice
So, how does this look in the real world? Imagine a modern telehealth application. When you're building a secure platform for patient consultations, choosing the right HIPAA compliant video conferencing platforms is non-negotiable. That platform must encrypt the entire video stream to protect the privacy of the conversation.
At the same time, when the doctor prescribes medication during that call, the order is sent to the pharmacy using an FHIR-based API. This ensures the prescription data is transmitted securely and in a format the pharmacy's system can process instantly. This whole workflow—from the secure video call to the electronic prescription—is a perfect example of compliance and interoperability working together to create a connected, efficient, and truly secure patient experience.
Architecting Scalable and Secure Medical Systems
How do you design an app experience that can scale to meet the size of any user audience, all while fending off constant cyberattacks? The answer is in the architectural blueprint. You wouldn't build a skyscraper on a flimsy foundation, and medical applications are no different—they demand an architecture built from the ground up for resilience, security, and growth.
This is where the real work of software engineering in healthcare kicks in. It's all about choosing the right patterns to create systems that are both powerful and dependable. Without a solid plan, even the most innovative features will fail under pressure or, worse, expose sensitive patient data. Sticking to proven software engineering best practices isn't just a good idea; it's essential.
From Monoliths to Microservices
For a long time, software was built as a monolith—one single, massive block of code where every component is tightly wound together. Picture carving a statue from a single block of marble. It’s solid and simple at first, but changing one small detail means re-carving the whole thing. That’s a risky and incredibly slow process.
The modern approach flips this on its head with a microservices architecture. Imagine building that same statue with LEGO bricks. Each brick is its own separate service: one handles patient authentication, another manages appointment scheduling, and a third takes care of billing. You can swap out, update, or scale any single "brick" without touching the others.
This modularity is a game-changer for healthcare. It lets development teams innovate faster, deploy updates more safely, and scale specific functions as needed. If your scheduling service suddenly gets slammed with traffic, you can give it more resources without over-provisioning the entire application.
This flexibility also contains failures. If the billing service hits a snag, the rest of the app—like a doctor accessing patient records—keeps running smoothly. To get a better handle on this, check out our guide on microservices architecture best practices.
Layering Security into the Foundation
In healthcare, security can't be a feature you tack on at the end. It has to be woven into every single layer of the architecture from day one. A system that can scale is worthless if it's not secure. This means going way beyond basic passwords and firewalls to create a true "defense-in-depth" strategy.
Business leaders need to make sure their development teams are implementing these core security measures:
- End-to-End Encryption (E2EE): This ensures data is scrambled from the moment it leaves a user's device until it reaches its destination. No one in the middle—not even the service provider—can decipher the information.
- Multi-Factor Authentication (MFA): Adding a second step for verification, like a code sent to a phone, makes it exponentially harder for a bad actor to get in, even with a stolen password.
- Proactive Vulnerability Scanning: Don't wait for an attack. Regularly and automatically scan your codebase and infrastructure for known weaknesses to find and patch holes before they can be exploited.
- Strict Access Controls: This is all about the Principle of Least Privilege. Users and systems should only have access to the absolute minimum data required to do their job. A nurse, for example, has no reason to see the hospital's financial records.
By asking the right questions about these architectural and security choices, business leaders can ensure their healthcare software is built not just for today's needs but is ready for future growth and evolving threats.
Integrating AI to Enhance Patient Care
Artificial intelligence isn't some far-off concept from a sci-fi movie anymore. In medicine, it's a real-world tool that’s actively changing how things get done, from the front desk to the operating room. When we talk about software engineering in healthcare today, a huge part of the conversation is about using AI to comb through mountains of data and pull out life-saving insights.
This isn’t about replacing doctors. It’s about giving them supercharged tools to see more, know more, and ultimately improve patient outcomes.
Think about radiology. AI algorithms can sift through thousands of scans, flagging subtle signs of tumors that the human eye might miss. These systems essentially act as a second pair of expert eyes, which helps cut down on missed diagnoses and seriously speeds up the review process.
Real-World AI Applications in Healthcare
AI’s impact goes way beyond the diagnostic lab. Healthcare organizations are bringing in sophisticated models to solve some of their biggest headaches, transforming both operations and patient care at the same time. The objective here is to build systems that aren't just smart, but are practical and fit right into the daily grind.
Here are a few powerful examples of AI in action:
- Predictive Analytics for Disease Outbreaks: AI models can analyze huge streams of public health data to forecast potential disease outbreaks. This gives hospitals and public health officials a critical head start to get resources and campaigns ready.
- Personalized Treatment Plans: By processing a patient's genetic profile, lifestyle, and medical history, AI can suggest highly tailored treatment protocols. This is a big step toward making medicine more precise and effective for the individual.
- Automating Administrative Tasks: Let’s be honest, clinicians spend too much time on paperwork. AI-powered tools can take over routine work like medical coding, billing, and scheduling, freeing them up to focus on actual patient care.
The adoption rate is telling. Recent research shows that 22% of healthcare organizations are now using domain-specific AI tools. That’s a massive 7x jump from just a year ago. You can explore the full findings from Menlo Ventures to see just how fast the industry is moving.
Navigating the Challenges of AI Integration
As exciting as AI is, dropping it into a live clinical environment is anything but simple. This isn't your typical software rollout; the stakes are incredibly high, demanding careful engineering and constant oversight. To get past the hype, we have to tackle the real-world headaches of making AI safe, fair, and reliable.
The biggest hurdles usually come down to the data. AI models are only as smart as the data they learn from, and healthcare data is notoriously messy and often biased. If a model is trained on data from just one demographic, its predictions could be dangerously wrong for other groups of people.
Mitigating data bias isn't just a technical problem; it's an ethical imperative. Successful AI integration requires a relentless focus on fairness, transparency, and patient safety to ensure that these powerful tools reduce health disparities, not amplify them.
This means software engineers have to build rock-solid governance and monitoring systems around their AI models. You can't just deploy a model and walk away. It needs continuous validation to make sure its performance doesn't drift and to catch any unintended side effects before they can cause harm.
Putting AI to work successfully is not a one-and-done project. It takes meticulous planning, a deep understanding of clinical workflows, and a serious commitment to ongoing monitoring and refinement. When it’s done right, AI becomes an incredible force for good, turning raw data into intelligence that makes operations more efficient and—most importantly—saves lives.
How to Modernize Your App with Smart AI Management
Adding AI into your healthcare app is a lot more involved than just connecting to an API. Think of it like dropping a high-performance engine into a classic car. Without a new dashboard, sensors, and control system, you have no way to manage that power, check your fuel, or even know if it's running safely. This is why a dedicated AI management system isn't just a nice-to-have; it's a critical part of your tech stack.
Without a central command center, development teams quickly find themselves drowning in operational chaos. They're juggling different AI models, trying to track runaway costs, and making sure every single prompt is secure and effective. This kind of administrative drag doesn't just slow down innovation—it opens the door to massive financial and compliance risks, something you absolutely cannot afford in software engineering in healthcare.
From Chaos to Control with a Central Hub
Picture this: your development team is trying to manage hundreds of AI prompts scattered throughout your application. One team pushes an update to improve diagnostic suggestions, but another team is unknowingly still using an older, less accurate version. Suddenly, you have inconsistent outputs and a confusing user experience.
A smart management tool acts as that missing command center. It provides a structured, sane way to handle all the moving parts of AI integration, giving you the freedom to build new features responsibly.
The role of a software engineer is shifting from a hands-on coder to a guide and manager of AI-powered processes. This requires a higher level of strategic thinking and architectural design, ensuring AI is implemented safely and effectively.
By centralizing how you handle AI, you immediately de-risk your initiatives and build a solid foundation for future growth. You can see how this plays out in practice by looking at how AI can be thoughtfully applied across the entire patient journey.
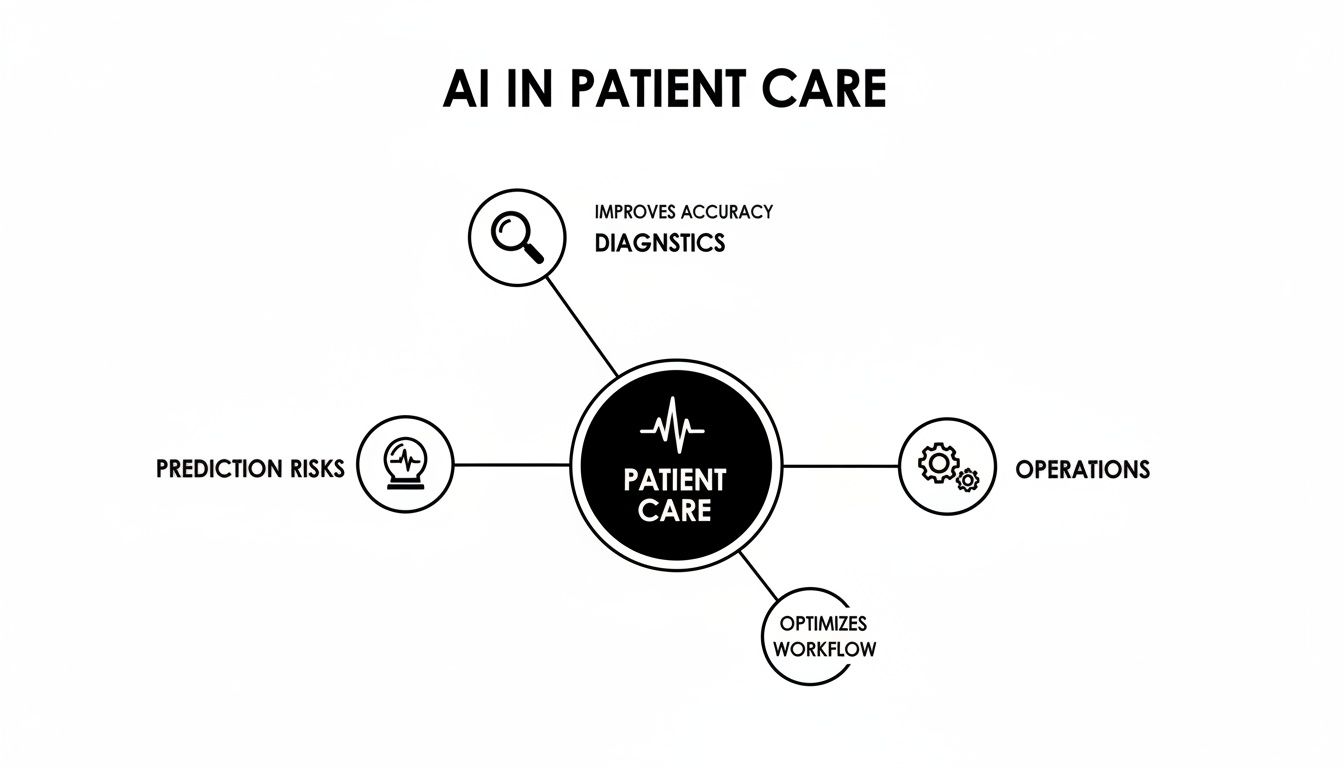
This map breaks down how a well-managed AI strategy can systematically improve everything from initial diagnostics to the efficiency of day-to-day operations.
Key Components of an AI Management System
A good system gives you the guardrails you need to build with confidence, turning AI integration from a high-stakes gamble into a predictable, scalable process. Wonderment has developed an administrative tool that developers and entrepreneurs can plug into their existing app or software to modernize it for AI integration.
Here’s what you should be looking for in a platform, like the one we’ve built at Wonderment:
- Prompt Vault with Versioning: This is your central library for every AI prompt. It lets you track changes over time, test out new versions, and instantly roll back if something doesn't work as expected. The result is consistency and quality across your entire app.
- Parameter Manager for Secure Data Access: This feature is all about control. You decide exactly what internal database information your AI models can see and use. It’s an essential security layer for protecting PHI while still letting the AI give you helpful, context-aware answers.
- Comprehensive Logging System: Every single interaction across all integrated AI models is logged and monitored. This gives you a priceless audit trail for debugging problems, analyzing performance, and proving compliance.
- Real-Time Cost Manager: AI API calls can get expensive—and fast. A cost manager gives you a live dashboard of your cumulative spend, allowing you to set budgets, see what's driving costs, and avoid any nasty surprises on your monthly bill.
By implementing this crucial management layer, you can speed up development, stay in control of your AI tools, and bring your application into the modern era responsibly. We are offering a demo of this powerful tool. It can transform your AI initiatives from a source of complexity into your greatest competitive advantage.
Building Your Healthtech Dream Team
A breakthrough medical app isn't a solo mission. It's brought to life by a highly specialized team that’s fluent in both code and clinical care. For business leaders, learning how to pick the right developers for your app or software project is one of the most critical steps you'll take. You need a mix of technical wizards and people who genuinely get the pressures and workflows of a real-world clinical setting.
Building great healthcare software isn't just about hiring skilled coders; it's about assembling a crew that can navigate the industry’s tangled web of regulations and operational headaches. This is no place for generalists. Your team needs to be built for the specific challenges of the medical world, where patient safety and data security are everything.
The Key Roles You Can't Afford to Skip
Think of your team like a surgical unit. Every role is distinct, essential, and has to work in perfect sync with the others. If one piece is missing, the whole operation is at risk.
Your core lineup absolutely has to include:
- Product Managers with Clinical Insight: These are your translators. They need to live and breathe the daily realities of clinicians and patients to make sure the software solves actual problems, not create new ones.
- Engineers Fluent in Health Data Standards: Developers with real, hands-on experience in FHIR or HL7 are worth their weight in gold. They know how to build the bridges between different systems, which is the key to making data flow.
- DevOps Engineers for HIPAA-Compliant Infrastructure: This role is all about building and maintaining a secure, scalable, and compliant cloud environment. They're the guardians of your application's foundation.
- UX/UI Designers with Empathy: Designing for healthcare demands a deep well of empathy. The user experience must be dead simple and stress-free for everyone, from busy doctors to anxious patients.
A well-rounded team doesn't just ship features; they build trust. Each role is a piece of the puzzle in creating a product that's not just functional, but safe, reliable, and genuinely helpful.
In-House Team vs. Specialized Agency
One of the first big decisions you’ll face is whether to build your team from scratch or bring in a specialized agency. An in-house team gives you deep integration with your company culture, but it can be a slow and expensive process to find the right people.
On the other hand, a specialized agency hits the ground running with immediate domain expertise and a ready-made team, which can seriously speed up your timeline.
The money flowing into this space is massive, which just goes to show how central software engineering has become. Healthcare IT spending was valued at USD 312.9 billion globally and is on track to nearly triple to USD 981.2 billion by 2032. Even though the US healthcare sector is a $4.9 trillion industry, only about $65 billion goes to software, pointing to a huge opportunity for growth.
If you want to explore more insights on healthcare software development, you'll see just how big the market is. Picking the right team structure is your first step to carving out a piece of it.
Answering Your Questions
Building software for healthcare is a world of its own, with unique challenges and complexities. Let's tackle some of the most common questions that come up when navigating this space.
What Is the Single Biggest Challenge in Healthcare Software Development?
It’s the constant tightrope walk between innovation and compliance. You want to build amazing new features that help doctors and patients, but you absolutely must follow stringent laws like HIPAA that protect patient data.
In most industries, you can move fast and break things. In healthtech, a single data breach isn't just a bug—it can lead to crippling fines, lawsuits, and a total loss of trust from the people who rely on your software. This means security and privacy can't be an afterthought; they have to be baked into every decision, right from the very beginning.
How Does FHIR Differ from HL7 and Why Is It Important?
Think of it this way: HL7 is like a digital fax machine, and FHIR is like a modern API. Both are standards for getting health information from point A to point B, but they couldn't be more different in practice. HL7 has been the workhorse for decades, but it's often rigid and a headache for developers.
FHIR (Fast Healthcare Interoperability Resources) is the newcomer, built on the same web standards we use for everything else online. That makes it incredibly developer-friendly and much more flexible.
The real magic of FHIR is its power to tear down data silos. It creates a common language that lets a hospital's EHR, a patient's health app, and a pharmacy's prescription system all talk to each other effortlessly. That seamless communication is the key to providing truly coordinated, modern patient care.
What Skills Are Most Important for a Healthcare Software Engineer?
Of course, top-notch programming skills and cloud expertise are table stakes. But in healthcare, that's just the start. You absolutely need a deep understanding of data security and hands-on experience with regulations like HIPAA and interoperability standards like FHIR.
But the secret weapon? Empathy. It might sound soft, but it's the most critical skill of all. Having empathy allows an engineer to truly understand the chaotic daily life of a nurse or a doctor. It's what separates a tool that adds to their administrative burden from one that genuinely makes their job easier and improves a patient's life.
At Wonderment Apps, we live and breathe these complexities every day. Our specialty is building secure, intelligent, and scalable healthcare applications that just work. If you’re looking to bring your software into the modern era with a smart AI management system that controls costs and speeds up development, we're the team to help you do it.
Schedule a demo with our team today and let us show you how our expertise can turn your vision into a reality.